Diet to Prevent Diabetes
The BBC recently led its UK national news with a story about the National Health Service (NHS) launching a Diabetes Prevention Programme in conjunction with Public Health England and Diabetes UK. It plans to address the largely preventable disease of Type 2 diabetes which costs the NHS 10% of its annual budget – £10billion! Current trends point to 1 in 3 people being obese and 1 in 10 Type 2 diabetic in less than 20 years.
In my homeland of Australia it is no less alarming. 3.61 million Aussies have diabetes or pre-diabetes. It is Australia’s fasting growing chronic disease. And worldwide the figure currently stands at 366 million diabetics.

Yet the shocking truth is that Type 2 Diabetes Mellitus (T2DM) can be delayed or prevented in a huge 58% of cases.
T2DM is a chronic condition that occurs when the pancreas does not produce enough insulin and/or the insulin does not work effectively to meet the body’s needs – 85% of all diabetes cases are T2DM.
For many people, T2DM can go undiagnosed for many years as some individuals display no symptoms, whereas for others the symptoms occur gradually, including blurred eyesight, slow healing, tingling and numbness in the feet. The first sign may even be a serious complication of diabetes such as a heart attack.
Diet to Prevent Diabetes
The first line of approach for diabetes prevention is lifestyle changes, including following a nutritious eating plan, being physically active in as many ways as you can and having regular health checks, particularly if you are aged over 45 or have a family history of diabetes.
Many individuals progress onto requiring diabetes medication as well as insulin therapy. Given that one person is diagnosed every 5 minutes, it is important that we are made aware of the actions that can be taken to reduce this burden.
Few Quick Facts:
- Diabetes is the 6th highest cause of death by disease in Australia.
- Hypertension (high blood pressure) and cardiovascular risk (heart disease and stroke) is doubled and high blood fat readings are more likely. Close to 80% of people with diabetes will die from a heart attack or stroke!
- Polycystic Ovary Syndrome (PCOS), Gestational Diabetes, Impaired Fasting Glucose (IFG) and Impaired Glucose Tolerance (IGT) all put individuals at higher risk of developing T2DM.
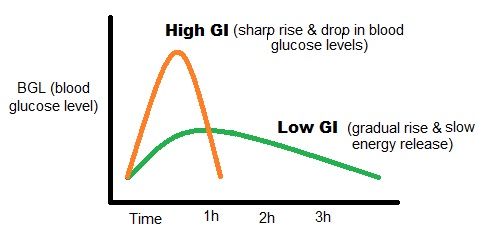
The Low Glycaemic Index (GI) Diet to prevent diabetes:
The amount of carbohydrate in a meal is a very important consideration in meal planning for people with diabetes. Contrary to popular belief, carbohydrates are not only found in the breads and cereals core food group (breads, cereals, rice, and pasta) and potatoes, but in all the 5 food groups, including vegetables (particularly potato, cassava and corn), meat alternatives (legumes), dairy (milk and yoghurt), and fruit. Looking at the GI alone is not adequate in predicting the effect of a food on blood sugar levels, but serves as a very useful starting point. Eating low GI foods in suitable portions will help you maintain consistent blood glucose levels. Low GI foods take longer to digest (particularly when protein, fibre or healthy fats are added), helping you to feel less hungry and assisting with weight loss/management.
To find out how much carbohydrates you should be consuming throughout the day as well as to plan a suitable diet to better manage your blood sugar levels, contact us.
Some low GI food choices:
Breads: Multigrain, sourdough, mountain
Cereals:muesli, oats and bran based 
Pasta and noodles: Wheat pasta (white and wholemeal)
Rice:Basmati, doongara
Grains: Pearl couscous, barley, semolina
Dairy: Reduced or low fat varieties
Legumes: All dried and canned beans, peas, lentils
Fruit: Most (watch out with portions of watermelon and grapes as these are easy to overeat)
Vegetables: Most, including sweet potato, yam and sweetcorn.
Summary of Healthy Eating Tips:
- Meal composition, quality and quantity are essential. Eating according to appetite a meal that contains high-fibre low-GI carbohydrates, good quality proteins, plenty of vegetables and healthy fats will improve the blood sugar readings after a meal.
- Regular meals with the incorporation of healthy snacks between meals (if you are hungry).
- Limit intake of unhealthy, saturated fats by choosing lean meats, low fat dairy, and avoiding fried or creamy restaurant and takeaway meals, desserts and processed snacks such as chips.
- Avoid alcohol, but if you choose to drink, limit it to 1-2 standard drinks per night and have at least 2 alcohol-free nights each week.
This article was originally published by Katherine Baqleh on WatchFit.
web sex livecam